
Heart Disease Is Failing Us

Heart Disease Definition
Any condition related to the heart is referred to as heart disease. The types are numerous, and some can be prevented.
Most people can prevent heart disease, even though it can be deadly. Choosing healthy lifestyle habits early could prolong your life and make your heart healthier.
Types of heart disease?
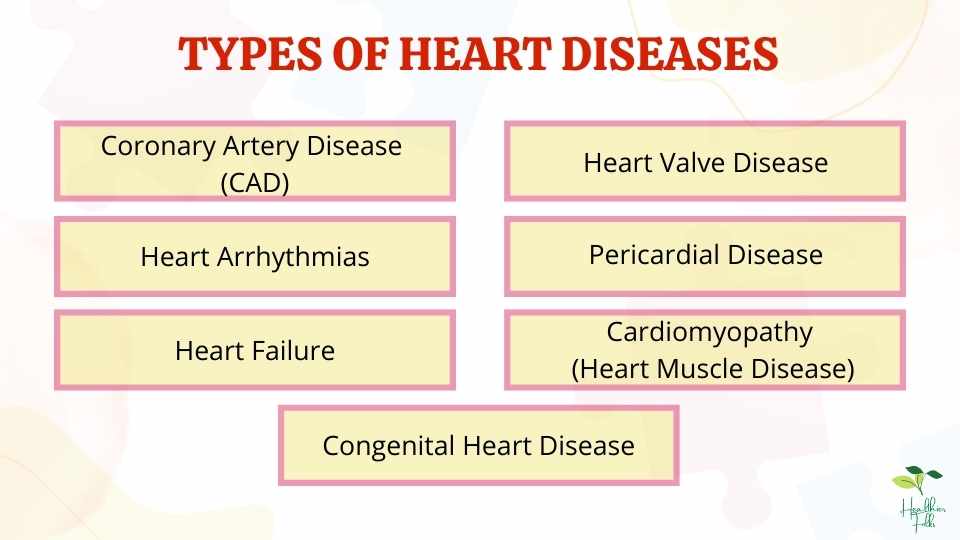
A wide range of cardiovascular problems can be classified as heart disease. The heart and blood vessels are affected in different ways by different types of heart disease.
Detailed information on some types of heart disease can be found in the sections below.
1. Coronary Artery Disease (CAD):
Definition: In the world, the most common heart disease is coronary artery disease (CAD). A blockage of your coronary arteries, which supply blood to your heart, may result from CAD. As a result, your heart muscle does not receive the oxygen it needs due to a decrease in blood flow. There is also a term for it: ischemic heart disease.
Atherosclerosis, which sometimes refers to the hardening of the arteries, is usually the main cause of the disease.
Symptoms of Coronary Artery disease are as follows:
- Chest pain, which is also known as angina, can sometimes occur
- It can cause a heart attack in some cases.
Risk factors
Coronary artery disease is caused by a number of different factors, including:
- Age: It may affect men after age 55 and women after menopause is mainly affected.
- Exercise: A lack of physical activity can result in triggering heart issues.
- Diabetes: Being diabetic or suffering from metabolic syndrome
- Family History: An inherited tendency to develop coronary heart disease in the family
- Genetics: All aspects of the cardiovascular system are controlled by genes, from the strength of blood vessels to communication between heart cells. Heart disease risk can be affected by genetic variations (mutations) in a single gene.
- High blood pressure: Blood supply to the heart is impeded by narrowed and damaged arteries due to high blood pressure. Angina, arrhythmias, and heart attacks can all result from insufficient blood flow to the heart.
- High levels of LDL or low levels of HDL: Plaque that clogs arteries is primarily caused by LDL cholesterol. HDL is responsible for clearing cholesterol from the body. The triglycerides in our bloodstream are another type of fat. In recent years, studies have also linked high triglyceride levels to heart disease.
- Obesity: People who are obese require more blood to oxygenate and nourish their bodies, causing their blood pressure to rise. To move this blood around, your body will also need to exert more pressure. Sadly, obese individuals are more likely to suffer from high blood pressure, which causes heart attacks.
- Smoking: Coronary arteries narrow and clog more quickly when you smoke. During this process, blood flow to the heart is reduced and heart attacks are more likely to occur.
- Stress: Hypertension and heart disease are caused by emotional stress, which increases blood pressure, and stress subsequently blocks coronary arteries.
2. Heart Arrhythmias.
Definition: Arrhythmias occur when your heart beats irregularly. There is a possibility that serious arrhythmias can occur on their own as well as develop from other heart problems.
Problems with heart rhythms (heart arrhythmias) occur when electrical signals coordinating heartbeats do not work correctly. Heartbeats that are fast (tachycardias), slow (bradycardias), or irregular are caused by faulty signaling.
Tachycardia: The word tachycardia (pronounced tak-ih-KAHR-dee-uh) refers to a fast heartbeat. Resting heart rate exceeds 100 beats per minute.
Bradycardias: The slowing of your heartbeat is known as bradycardia (pronounced brad-e-KAHR-dee-uh). In resting conditions, the heart rate is lower than 60 beats per minute.
Symptoms of Heart Arrhythmia are as follows:
- A racing heartbeat (tachycardia)
- A slow heartbeat (bradycardia)
- Fatigue/tiredness
- Pain in the chest
- Short breaths
- Dizziness
- Sweating
- Feeling faint
- Anxiety
Risk factors
Heart Arrhythmia is caused by a number of different factors, including:
- Congenital heart disease: When you are born with a heart condition, your heart can have irregular rhythms.
- Previous heart surgery and coronary artery disease: Heart conditions such as narrowed arteries, heart attacks, abnormal valves, heart failure, cardiomyopathy, and other heart damage increase the risk for arrhythmias.
- High blood pressure: Coronary artery disease is more likely to develop due to high blood pressure. The left lower chamber of the heart (left ventricle) may also become stiff and thick, altering how electrical signals are transmitted.
- Obstructive sleep apnea: As a result of obstructive sleep apnea, you experience pauses in breathing while you sleep. Symptoms include a slow or irregular heartbeat (bradycardia), as well as atrial fibrillation.
- Thyroid disease. It is possible to experience irregular heartbeats if your thyroid gland is overactive or underactive.
- Electrolyte imbalance: Heart electrical impulses are triggered and sent by electrolytes in the blood, such as potassium, sodium, calcium, and magnesium. Heart rate and rhythm may be affected if electrolytes are imbalanced, for example, if the levels are too low or too high.
- Caffeine, nicotine, or another drug use: You can develop more serious arrhythmias if you consume caffeine, nicotine, and other stimulants. Many types of arrhythmias and sudden deaths can be caused by illegal drugs, such as amphetamines and cocaine.
- Certain drugs: Arrhythmias can be caused by certain prescription medications and cough and cold medications obtained without a prescription.
- Excessive alcohol consumption: A heart condition called atrial fibrillation can be caused by too much alcohol consumption. Alcohol can affect electrical impulses in your heart.
3. Heart Failure.
Definition: Long-term heart failure, also called congestive heart failure, is an illness that worsens over time. In spite of what its name suggests, heart failure refers to a problem with your heart’s ability to pump blood. You can suffer damage to your organs and accumulate fluid in your lungs when your heart pumps less efficiently.
Symptoms of Heart Failure are as follows:
- Feeling short of breath.
- Fatigue or feeling tired most of the time
- Swelled body parts like the abdomen, ankles, and legs
- An increase in weight.
- During sleep, the urge to urinate arises.
- Fast or irregular heartbeats
- A dry cough or wheezing
- Upset stomach and feeling of nausea.
Risk factors
Heart Failure is caused by a number of different factors, including:
- Heart attack and coronary artery disease: Heart failure is most often caused by coronary artery disease, which is the most common form of heart disease. In this condition, fatty deposits build up in arteries, reducing blood flow and resulting in heart attacks.
Coronary arteries become completely blocked suddenly during a heart attack. A heart attack may damage your heart muscle, affecting your heart’s ability to pump
- High blood pressure: To circulate blood throughout your body, your heart must work harder if your blood pressure is high. With repeated exercise, your heart muscle can grow stiff and weak, making it hard to pump blood properly.
- Faulty heart valves: Keeping the blood flowing properly is the job of the valves in the heart. As a result of a damaged valve or coronary artery disease, the heart must work harder, causing the heart to weaken.
- Age: With advancing age, there is an increased risk of heart failure. Among people over 65 years of age, heart failure is often the cause of hospitalization.
- Family History and Genetics: Heart failure is more likely to develop in people with a family history of cardiomyopathies. Heart failure risk gene variants are under investigation by researchers.
- Diabetes: Diabetes, combined with coronary artery disease and high blood pressure, puts a person at high risk for heart failure. Heart failure may be exacerbated or caused by some diabetes medications, such as rosiglitazone and pioglitazone. It is also associated with an increased risk of heart failure in patients with chronic kidney disease due to diabetes.
- Obesity: A person’s risk of heart failure is increased if they are obese because obesity increases blood pressure and diabetes type 2. Women are particularly at risk for heart failure due to obesity according to the studies.
- Lifestyle Factors: Heart failure can be caused by smoking, sedentary lifestyles, alcohol abuse, and drug abuse.
- Heart failure medications: The heart can be damaged by certain medications, resulting in heart failure. High-dose anabolic steroids increase heart failure risk over time.
4. Heart Valve Disease.
Definition: Heart valve disease is a condition that causes one or more of your heart’s valves to malfunction. In the absence of treatment, heart valve disease can result in your heart working harder. Depending on the severity of the condition, it may even endanger your life. Your healthcare professional can repair or replace your heart valves in many cases through surgery or a minimally invasive procedure, restoring normal function and allowing you to return to your normal activities.
Blood flows through your heart only in one direction due to the four heart valves. There are four types of valves in your heart:
- Mitral valve: The mitral valve is located between the left atrium and left ventricle.
- Tricuspid valve: The tricuspid valve is located between the right atrium and right ventricle.
- Aortic valve: The Aortic valve is located between your left ventricle and aorta.
- Pulmonary valve: The Pulmonary valve is located between your right ventricle and pulmonary artery.
Symptoms of Heart Valve Disease are as follows:
- Short breaths
- Chest pain
- Fatigue
- Irregular heartbeat
- Shortness of breath, particularly when active or lying down
- Swelling of your abdomen, ankles, and feet
- Quick weight gain.
- Dizziness or weakness
- Fainting
Risk factors
Heart Valve Disease is caused by a number of different factors, including:
- Rheumatic Fever: Strep throat and rheumatic fever are caused by the same bacteria. Individuals who do not get treated for their strep throat infection are most likely to suffer from this condition. During rheumatic fever, your body can damage your heart muscle and valves, causing your valves to narrow or leak. A person with rheumatic fever might not experience symptoms of heart valve damage for 10 to 20 years after the infection.
- High Blood Pressure: The pressure within your arteries is caused by the pressure exerted by your blood. High blood pressure over a long period of time can increase the size of your heart or your main arteries, which can lead to heart valve problems.
- Endocarditis: The endocardium is the lining of your heart’s valves and chambers. Endocarditis occurs when the endocardium becomes infected. There are usually bacteria or fungi responsible for it. Heart valve disease can still develop after you’ve been treated with antibiotics for several weeks for endocarditis.
- : Older adults are more likely to suffer from heart valve conditions. Valve degeneration and deterioration are common as you age. Calcium deposits can sometimes build up on your valves. Further, this may result in prohibiting your valves from working in an accurate way.
- Heart Conditions: Heart valve disease is more likely to occur in people with a history of other heart problems. Heart attack victims usually have damaged heart muscle, which affects the heart valves, after they have suffered a heart attack or other heart issues. It is also possible to develop heart valve disease if you were born with a heart condition.
5. Pericardial Disease.
Definition: Pericarditis, a condition in which your heart’s outer surface is coated with fluid, is an inflammation of the pericardium. As a result of sudden inflammation or injury of the heart, pericarditis can last from a few weeks to several months. Some attacks can last for years, while others clear up after three months.
Symptoms of Pericardial Disease:
- Pain behind the breastbone or on the left side of the chest
- Coughing
- Fatigue or weakness
- Swelling in the abdomen, legs, and ankles
- Low-grade fever
- Heart palpitations
- Shortness of breath
Risk factors
Pericardial Disease is caused by a number of different factors, including:
- Past heart conditions: The past experience of a heart attack
- The autoimmune disease
- Trauma or injury: Accidental trauma or injury
- Infections: Certain viral, bacterial, and fungal infections can result in pericardial disease
- Kidney failure
- Certain medications
6. Cardiomyopathy (Heart Muscle Disease)
Definition: Cardiomyopathy is a condition that affects the heart muscle. Scar tissue can form in the heart as a result of cardiomyopathy, which causes your heart to stiffen, enlarge or thicken. As consequence, your heart cannot pump blood efficiently.
Heart failure can result from cardiomyopathy over time. Treatment can help. A heart transplant may be necessary for some people with cardiomyopathy.
Symptoms of Cardiomyopathy (Heart Muscle Disease):
- Shortness of breath
- Fatigue.
- Heart palpitations.
- Fainting
- Swelling in the calves, legs, or ankles.
Risk factors
Cardiomyopathy (Heart Muscle Disease) is caused by a number of different factors, including:
- Heart attacks or coronary artery disease (CAD).
- Family history of heart failure
- Autoimmune diseases
- high cholesterol diseases
- Heart attacks in the past.
- Pregnancy.
- Diabetes and thyroid problems are diseases affecting the endocrine system.
7. Congenital Heart Disease.
Definition: Heart problems that are present since birth are called congenital heart disease. The term congenital refers to a condition that is present at birth. During childhood and adulthood, congenital heart disease can alter the flow of blood through the heart.
The severity of congenital heart disease can vary depending on the type. There is a risk of life-threatening complications in complex defects, however. Congenital heart disease survival, however, continues to improve as diagnosis and treatment progress.
Symptoms of Congenital Heart Disease:
- Blue skin, lips, and fingernails
- Irregular heart rhythms (arrhythmias)
- Swelling of body organs
- Shortness of breath
- Feeling tired very quickly with physical activity or Fatigue
Risk factors
Congenital Heart Disease is caused by a number of different factors, including:
- Genes. There is an inherited tendency for congenital heart disease. Numerous genetic syndromes are linked to it.
- Medications. Birth defects can occur as a result of taking certain medications during pregnancy. Isotretinoin (Claravis, Myorisan, others), used to treat acne, and lithium, used to treat bipolar disorder, has been linked to heart defects. Be sure to discuss your medications with your health care provider.
- Alcohol. Alcohol consumption during pregnancy can lead to heart defects in the unborn child.
- Smoking. Getting rid of cigarettes is the best thing you can do. Pregnant women who smoke are at greater risk of their babies developing congenital heart defects.
Prevention of Heart Diseases
1. Avoid smoking and using tobacco:
Smoking and using smokeless tobacco are both damaging to your heart.
2. Get moving:
Exercise helps you maintain a healthy weight. This, help in reducing the heart disease risk.
3. Healthy diet:
Type 2 diabetes is reduced when you eat a healthy diet. Diet (including healthy meals) can reduce blood pressure, cholesterol, and blood sugar.
4. Healthy weight maintenance:
A person who is overweight may develop high blood pressure, high cholesterol, and type 2 diabetes, which can increase their chances of developing heart disease. Hence, one should maintain a healthy weight.
5. Quality sleep:
Sleep deprivation increases the risk of obesity, heart attacks, high blood pressure, diabetes, and various mood disorders or depression.
6. Stress management:
People sometimes cope with stress by overeating, drinking, or smoking which are considered as wrong ways. However, exercise and meditation can help improve your health by helping you manage stress.
Diagnosis of Heart Diseases
Heart disease can be diagnosed using a variety of tests. To diagnose heart disease, in addition to blood tests and chest X-rays, the following tests may be done:
- Electrocardiogram (ECG or EKG). In an ECG, electrical signals in the heart are recorded quickly and painlessly. If the heart beats too fast or too slowly, it can detect it.
- Holter monitoring. During daily activities, a Holter monitor records the heart’s activity over the course of a day or more.
- Echocardiogram. A sound wave can be used to create a detailed image of the heart’s motion during this noninvasive procedure.
- Exercise tests or stress tests. It is possible to determine if heart disease symptoms are present during exercise by undergoing exercise tests.
- Cardiac catheterization. Heart artery blockages can be detected by this test.
- Heart (cardiac) CT scan. Cardiovascular CT scans are performed inside a doughnut-shaped machine while you lie on a table. Images of your heart and chest are collected by rotating an X-ray tube inside the machine.
- Heart (cardiac) magnetic resonance imaging (MRI) scan. Cardiovascular MRIs use computer-generated radio waves and a magnetic field to generate detailed heart images.
Treatment of Heart Diseases
Lifestyle Changes
Lifestyle changes can reduce the risk of heart disease – or even prevent it entirely. To improve heart health, make the following changes:
- Avoid Smoking
- Keep a check on blood pressure
- Consume healthy meals
- Take routine cholesterol test
- Keep a check on diabetes
- Physical activity or Exercise
- Stress Management
- Improved Sleep
The type and cause of heart damage determine the treatment of heart disease.
Medications
To control heart disease symptoms and prevent complications, medications may be needed if lifestyle changes do not work. There are different types of heart diseases that require different types of medication.
Procedures involving surgery
Depending on the severity of the heart disease, some people may need surgery or a procedure.



